AI is rewriting how doctors read ECG

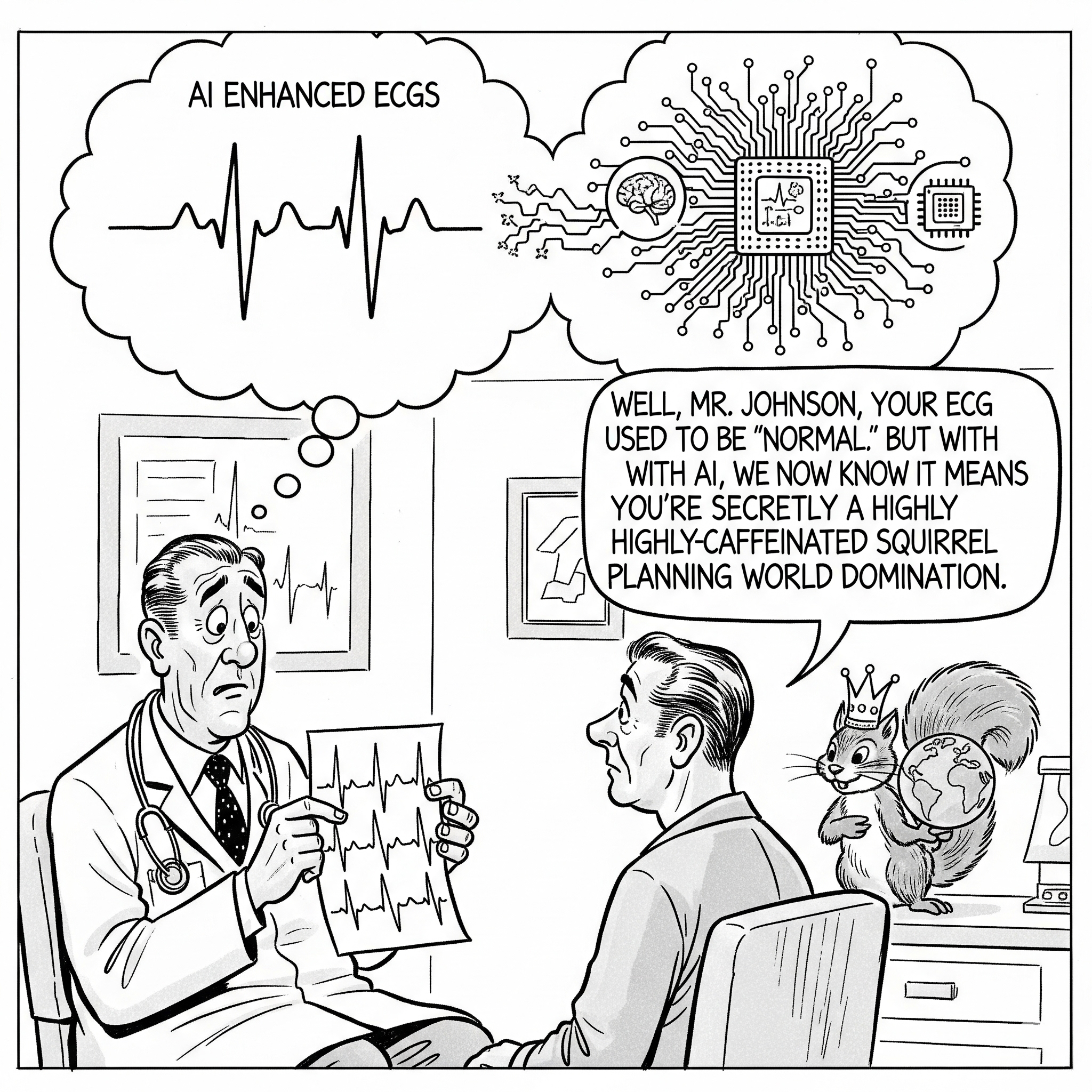
A new kind of mind is revealing secrets hidden in plain sight, challenging a century of medical wisdom and rewriting the rules of cardiovascular diagnosis. It's not a new stethoscope or an innovative imaging machine. It's a deep-learning AI, and its canvas is a piece of medical history: the humble electrocardiogram, or ECG. For more than a hundred years, we thought we knew everything there was to know about the squiggly lines on an ECG, but it turns out, we were missing the forest for the trees.
The story of the electrocardiogram is one of quiet, unwavering utility. Since its invention by Willem Einthoven in the early 20th century—an innovation that earned him a Nobel Prize—the ECG has been the bedrock of cardiovascular medicine. It's a snapshot of the heart's electrical activity, a quick and painless test that can reveal heart attacks, arrhythmias, and other acute problems. We've become so comfortable with it that its signals, like Morse code, are read and interpreted by doctors and machines alike. But for all its brilliance, the ECG has always been viewed as a series of specific, discernible patterns. A certain spike here means one thing, a dip there means another. The wisdom of cardiology has been built on this bedrock of discrete, interpretable findings.
And yet, this established wisdom has a blind spot. What if the most crucial information isn't a single, dramatic spike but a symphony of subtle, non-linear patterns, a kind of subliminal message hidden in the noise? This is precisely the question a team of researchers from Yale University and the Amsterdam University Medical Centre set out to answer, and their findings are nothing short of revolutionary. Using artificial intelligence, they've shown that AI-enhanced ECGs—or AI-ECGs—aren't just better at spotting specific diseases; they've effectively redefined what an abnormal ECG means.
The researchers, led by Philip M. Croon and Lovedeep S. Dhingra, and senior author Rohan Khera, started with a simple hypothesis: AI-ECG models, trained to detect a specific condition like left ventricular systolic dysfunction (LVSD), might be picking up on something more general than just that one disease. The established view is that each model is a condition-specific classifier. In the world of AI, this is known as a supervised learning problem. You show the model thousands of examples of ECGs from people with a specific disease, and thousands from people without it, and it learns to distinguish between them. It’s like teaching a child to recognise a cat by showing them pictures of cats and dogs. In this study, the "cats" were cardiovascular diseases like aortic stenosis (AS), mitral regurgitation (MR), and left ventricular hypertrophy (LVH), and the "dogs" were healthy controls.
The team leveraged a sophisticated AI model known as a convolutional neural network (CNN), specifically the EfficientNet-B3 architecture. A CNN is a type of deep-learning AI that's particularly adept at analyzing images, which is exactly how these researchers fed the ECG data to the model—as 300x300 pixel images of the squiggly lines. This isn't just a clever formatting trick; it allows the AI to see the ECG not as a set of discrete measurements but as a whole, holistic visual pattern, much like a radiologist sees an X-ray. The CNN, with its 384 layers and over 10 million trainable parameters, can find connections and patterns that are simply invisible to the human eye, no matter how experienced.
And what the AI found was astonishing. The models, despite being trained on specific, narrow disease labels, were not acting as specialised detectives. Instead, they behaved like a general alarm for cardiovascular trouble. In a study of over 230,000 individuals across four diverse populations in the US and UK, the researchers found that an AI-ECG model trained to detect a single condition, like LVSD, was also highly effective at identifying a broad range of other heart diseases. The findings were consistent across all cohorts, including the UK Biobank, a large, prospective study of generally healthy individuals.
This is the "emperor's new clothes" moment. Cardiologists have long looked at ECGs and seen only what they were trained to see—specific, well-defined abnormalities. But the AI, unburdened by this historical bias, was able to see the subtle, collective signature of a heart under stress, regardless of the specific diagnosis. It was as if the AI was saying, "That heart is sick, but it's not just sick with one thing. It’s sick with a general, underlying cardiovascular vulnerability that manifests in many ways."
The implications of this finding are profound. This isn't just an incremental improvement on an old tool; it’s a reframing of its entire purpose. The paper argues that AI-ECGs should no longer be viewed as "binary diagnostic tools" for specific conditions but rather as "broader cardiovascular biomarkers". A positive screen, regardless of the model used, should trigger a comprehensive evaluation that goes beyond the single disease it was trained to detect. This is particularly important for healthcare systems like the NHS, where resources are often stretched thin and a quick, reliable screening tool could save lives by identifying at-risk individuals early.
This new tool, however, is not a replacement for a clinician's expertise. It's a new layer of information, a digital biomarker that can guide clinical decisions. In a world where patients often present with multiple, co-existing conditions, an AI-ECG that signals a general state of cardiovascular distress is arguably more useful than one that can only spot a single, isolated problem. This is a game-changer for preventative medicine. A patient with a high AI-ECG score, even without overt symptoms, could be a candidate for more aggressive preventive strategies like intensified blood pressure control or lipid-lowering therapies, effectively getting ahead of a problem before it becomes a crisis. The study also highlighted that the ensemble model, which was trained to detect a composite of structural heart diseases, showed stronger and broader associations than the single-condition models. This suggests that the future of AI-ECG lies in the development of tools designed for broad, holistic screening rather than narrow diagnostics.
But this new era of AI-driven discovery also brings with it new challenges. The concept of an "algorithmic divide" is a very real concern. The effectiveness of these AI models is entirely dependent on the data they are trained on. The study population was diverse, including cohorts from a large tertiary hospital, community hospitals, an outpatient network, and the UK Biobank. However, if an AI is trained primarily on data from one demographic group, say, predominantly white populations, it may not be as effective in detecting disease in others. The study acknowledged that the UK Biobank cohort, for example, was 96.6% White, which could potentially limit the generalisability of some findings. This isn't just a technical problem; it's a social justice issue. The power of these new tools must be applied equitably, or they will simply amplify existing health disparities.
In the end, the story of AI-ECG is a powerful parable about seeing the world in a new way. For decades, we've treated the ECG as a series of specific, discrete signals. But AI, with its capacity to find subtle, hidden connections, has revealed it to be something much more. It's not a list of diagnoses; it's a window into the overall health of the cardiovascular system. In a world where one of the most powerful tools in medicine is also one of the oldest, this new perspective is not just interesting—it could be a matter of life and death. The doctor may have seen your ECG, but now, a new kind of mind is seeing it, too, and it’s seeing things we never even knew were there.
Comments ()